Beijing Tiantan Hospital researchers pioneer one-stage hybrid surgery for brain and spine tumors
Neurosurgeons combine embolization and resection in a single procedure for safer outcomes in hypervascular CNS tumors
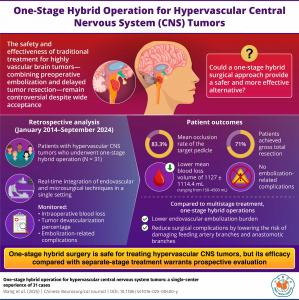
BEIJING , CHINA, August 21, 2025 /EINPresswire.com/ -- Hypervascular tumors of the central nervous system (CNS), including meningiomas, hemangioblastomas, and paragangliomas, remain among the most challenging lesions encountered in neurosurgery. These tumors are characterized by a dense vascular network that complicates surgical removal, often obscuring anatomical boundaries and significantly increasing the risk of heavy intraoperative bleeding. This in turn can prolong operative time, impair visibility, and elevate the potential for neurological injury. For decades, the conventional management approach has involved a two-stage process in which preoperative embolization is carried out to block blood supply to the tumor, followed days later by microsurgical resection. While this method has been widely used, it carries notable drawbacks such as post-embolization swelling, hemorrhage, and the risks associated with a delay between procedures. As a result, outcomes are variable, and the staged technique is not universally suitable for every patient.In response to these limitations, neurosurgeons at Beijing Tiantan Hospital explored whether performing endovascular embolization and surgical removal in a single session could offer a safer and more efficient alternative. This method, termed a one-stage hybrid operation, was applied and refined over a decade of practice at the institution. In their recently published study, the team presented the results of 31 patients treated between 2014 and 2024, representing one of the most comprehensive clinical series of its kind. The findings were published in the Chinese Neurosurgical Journal on July 31, 2025, in Volume 11, Article 14, and they highlight how combining two complex procedures into a single integrated workflow can transform patient care.
Patients in the study represented a broad clinical spectrum, ranging from young adults to seniors. Tumors were located in particularly challenging sites, such as the skull base, cerebellum, and brainstem—areas where surgical access is narrow and delicate neural structures are at constant risk. Despite these difficulties, the outcomes were striking. Gross-total tumor removal was achieved in 71 percent of patients, with near-total resection in 19.4 percent and partial removal in 9.7 percent. Perhaps most importantly, the average blood loss during surgery was more than 1,100 mL lower than what is typically observed in conventional staged cases. This reduction in intraoperative bleeding not only simplified the operative field but also improved overall safety for the patient. Equally significant was the absence of embolization-related complications, a concern that often deters surgeons from more aggressive endovascular strategies.
Postoperative outcomes further underscored the value of the hybrid method. At the time of discharge, 87 percent of patients demonstrated stable or improved neurological function compared to their preoperative status. Follow-up at 12 months revealed that two-thirds of patients were symptom-free, pointing toward both short-term safety and longer-term durability of the treatment. These results suggest that combining embolization with immediate resection can reduce surgical risks while preserving neurological integrity. According to Professor Yi Lu, who led the research team, “There is an urgent need for an innovative solution that can achieve both vascular obliteration and elimination of complications.”
The technical approach adopted at Beijing Tiantan Hospital was meticulous. During the embolization phase, surgeons targeted deep or surgically inaccessible feeding arteries that posed the highest risk of uncontrollable bleeding. In contrast, more superficial vessels were deliberately left intact so they could be directly managed during the resection phase. This selective embolization strategy helped maintain normal perfusion in adjacent brain tissue, thereby reducing the likelihood of ischemic complications. Materials used included ethylene vinyl alcohol copolymer (EVOH), detachable coils, and silk suture fragments, each chosen for its capacity to provide targeted and durable occlusion. In specific cases where control of blood flow was essential during craniotomy, balloon catheters were used to temporarily regulate circulation, giving the surgical team additional time and precision.
The procedures were conducted in a specially designed hybrid operating room equipped for both endovascular interventions and open neurosurgery. This environment allowed the team to transition seamlessly from embolization to tumor resection without the need to shift the patient between suites or interrupt anesthesia. Such continuity not only reduced surgical duration but also minimized risks related to repeated induction and recovery. The ability to carry out both procedures under a single anesthesia further lowered the psychological and physical stress experienced by patients and their families.
The clinical implications of this innovation are considerable. By unifying two complex procedures into one, the hybrid approach reduces the cumulative risks associated with staged treatment and offers a new level of safety for tumors traditionally considered high risk. It also opens the door for broader application to other hypervascular CNS lesions where bleeding remains the primary obstacle to effective surgical management. According to Professor Li, a co-author of the study, “Our experience suggests that the one-stage hybrid operation is safe for the treatment of hypervascular CNS tumors.”
Nevertheless, the researchers emphasize the importance of cautious optimism. While the results from their single-center experience are compelling, larger multicenter studies are necessary to validate the superiority of this method over conventional staged approaches. Prospective trials comparing outcomes directly between the two strategies will be crucial for determining whether the hybrid method should be adopted as a new standard of care worldwide. Until such data are available, the one-stage hybrid procedure represents a promising yet still emerging solution.
Taken together, the findings of this study mark a meaningful step forward in the surgical management of hypervascular brain and spinal tumors. By addressing long-standing limitations of staged surgery and demonstrating consistent improvements in blood loss, neurological outcomes, and patient recovery, Beijing Tiantan Hospital has provided evidence that may reshape neurosurgical practice in the years to come.
***
References
Title of original paper: One-stage hybrid operation for hypervascular central nervous system tumors: a single-center experience of 31 cases
Journal: Chinese Neurosurgical Journal
DOI: https://doi.org/10.1186/s41016-025-00400-y
About the University
Beijing Tiantan Hospital is a leading center for neurology and neurosurgery in China, renowned for its clinical expertise and research excellence. Affiliated with Capital Medical University, the hospital provides advanced care in the diagnosis and treatment of neurological diseases, and is recognized internationally for pioneering surgical innovations and contributions to neuroscientific research.
Website: https://cbtn.org/institutions/beijing-tiantan-hospital-neurosurgery-center-beijing-china
Yi Lu
Beijing Tiantan Hospital
+861059978478 ext.
luyi617@sina.cn
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the author above.